Browse through our photo gallery of various throat disorders we have worked with over the years. For detailed descriptions on each disorder, click here.
Note: For a much larger gallery of photos, see our new standalone educational website, Laryngopedia.
Ulcerative supraglottitis. This form is an atypical, extremely painful, but less fulminant case, possibly viral in origin (Lab).
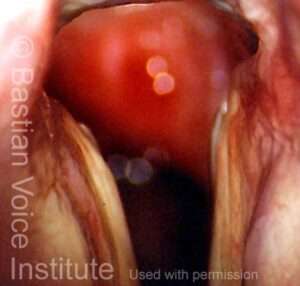
Cancer involving the supraglottic larynx. The airway (dark area) and vocal fold are partially obscured by out-growing tumor (Lab).
Vascular prominence (capillary ectasia) (Lab).
Open epidermoid cyst. Note mottled appearance, white color of cyst contents, bilaterality, and small divot at arrow showing point of leakage but not complete emptying of cyst contents (OR).
Large glottic web comprising most of the vocal folds, after removal of large smoker’s polyps and surgeon-directed voice rest for 21 days (Lab).
Intubation injury at posterior commissure. Note that the posterior portion of each fold has a divot or “cookie bite” where the breathing tube created pressure necrosis (Lab).
Left mucus retention cyst with right nodular reaction (OR).
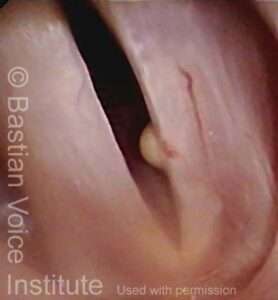
Small mucus retention cyst and capillary ectasia, left vocal fold. Note yellowish color and origin from just below free margin, as well as normal right vocal fold (Lab).
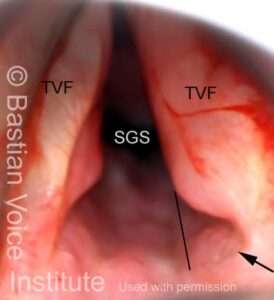
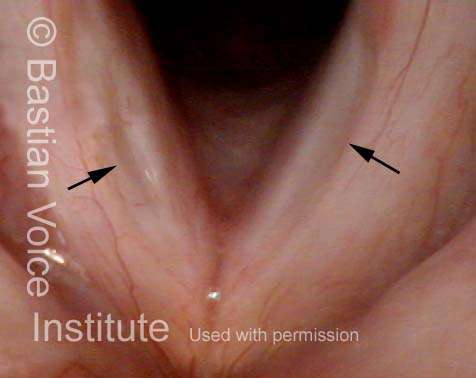
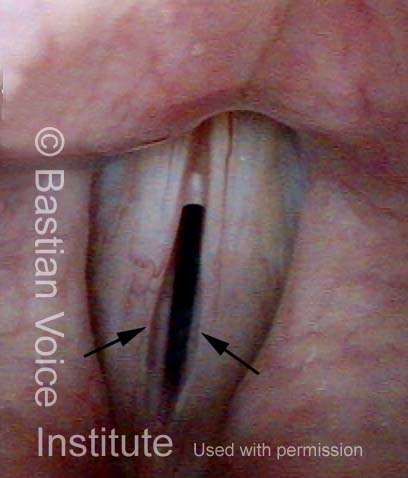
Severe injury from prolonged intubation. There are divots at posterior 1/3 of each vocal fold. Thin dark line demonstrates expected continuation of fold, to accentuate the divot (small black arrow). Subglottic stenosis seen faintly in the receding darkness below the folds (OR).
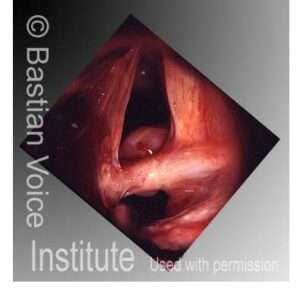
Posterior commissure synechia after prolonged intubation. The posterior part of the vocal folds are tethered together, preventing full opening during breathing (OR).
Left anterior saccular cyst (Lab).
Papillomas in patient with recurrent respiratory papillomatosis (RRP) involving subglottis and very high trachea (Lab).
Tracheal stenosis seen below the vocal folds in the high trachea. This may be caused rarely by injury from long-term breathing tube, tracheotomy, blunt trauma, or other influences (Lab).
Bilateral moderate-sized nodular swellings. Left larger than right; whitish discoloration left is mucus (Lab).
Candidia
Candida infection of the vocal folds, often caused by inhalation of aerosolized steroid for asthma. Usually seen with higher strengths of medication and frequent dosing; also more likely if antibiotics used at same time (Lab). This can look like mucus accumulation, but does not move or clear away even with aggressive throat-clearing.
Same patient, after treatment with antifungal agent. Note residual haziness (Lab).
Contact Granuloma
Epidermoid Cyst
Right epidermoid cyst during breathing (Lab). Note whitish sphere not as prominent due to thicker overlying mucosa, vascularity and mucus, suggesting concurrent acid reflux.
Same patient, during phonation, showing mismatch. In addition, right side very stiff and non-vibratile (Lab).
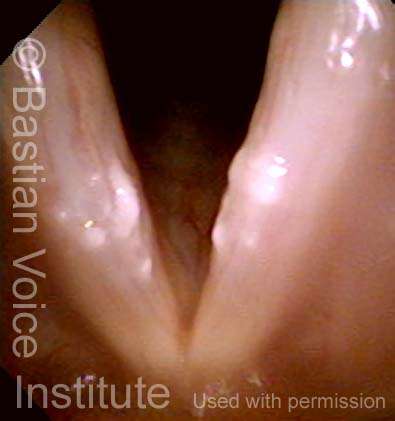
Glottic Furrow
Glottic furrow (vergeture), breathing vocal fold position, resembling a furrow in a recently-plowed field (Lab).
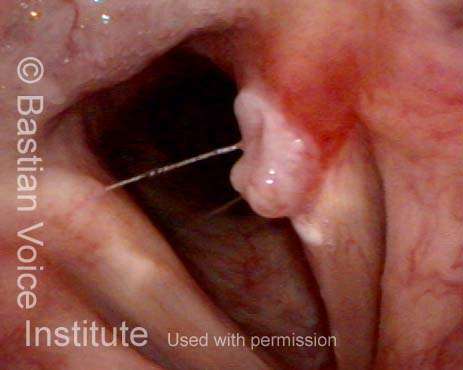
Same patient during phonation. Such patients may have a lot of bowing as a concomitant finding, but the two edges of the furrow are seen on each fold, at arrows (Lab).
Vocal Fold Hemorrhage
Diffuse resolving hemorrhage (bruise) right vocal fold and bilateral moderate nodular swellings. White material is mucus that goes away with throat clearing—suggesting acid reflux (Lab).
Same patient in open, breathing position of folds.
Hemorrhagic Polyp
Subglottic Stenosis
Laryngitis Sicca
Glottic Sulcus
Glottic Cancer
Early right vocal fold carcinoma, operative view (OR).
Same lesion, at the start of laser removal (OR).
Same larynx, after removal is complete. With healing over the next several months, the deficit “fills in” and voice result is often surprisingly good (OR).