Disorders Treated
Bastian Voice Institute is a full-service laryngology practice that has a particular focus on and experience with a variety of voice, swallowing, airway, and coughing disorders.

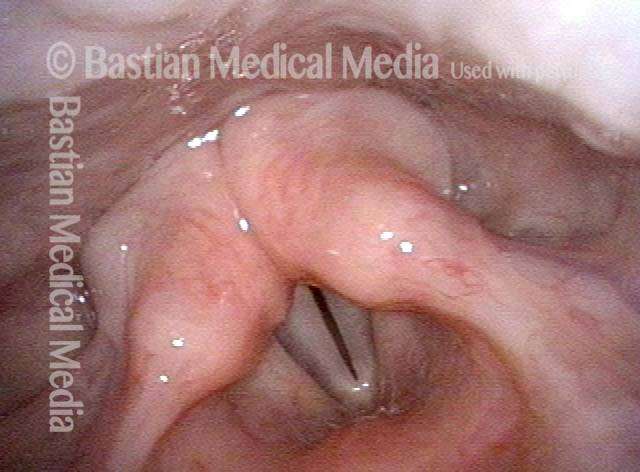
Vocal Fold Injuries
Lesions (abnormal tissue) on the surface tissue of the vocal folds, typically caused by vocal overuse. These include:
- Nodules (pictured)
- Polyps
- Capillary ectasia
- Epidermoid cysts
- Glottic sulcus
- Smoker’s polyps

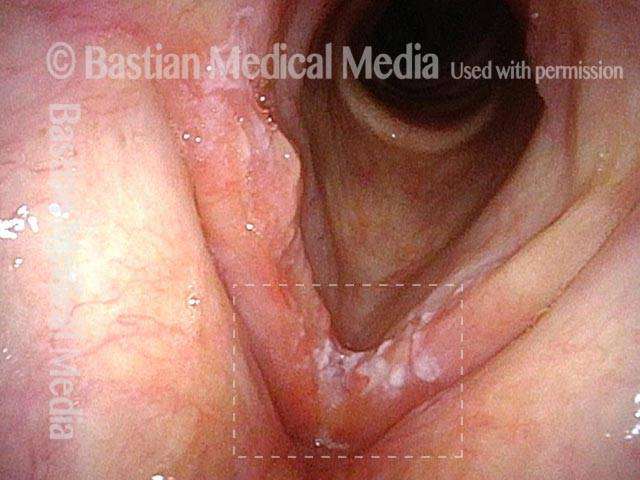
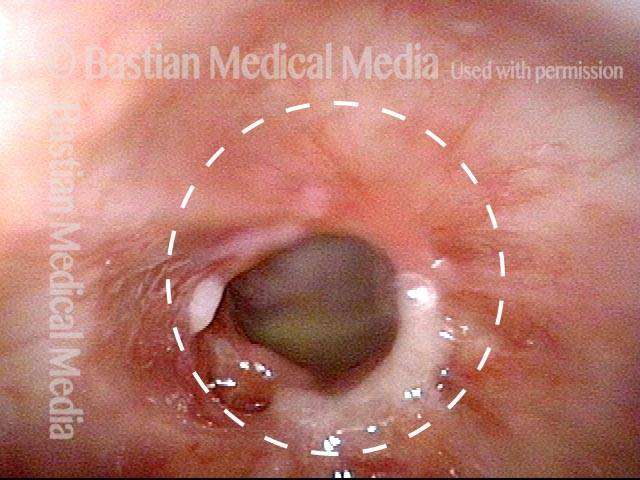
Other Benign Lesions and Conditions of the Larynx
Lesions or conditions that arise in the larynx but, unlike vocal fold injuries, usually without correlation to voice use. These include:
- Contact or intubation granulomas
- Mucus retention cysts (pictured)
- Saccular cysts
- Laryngopharynx acid reflux
- Laryngitis
Benign vocal fold lesions
Lesions of the mucosa — the glistening, wet surface covering of the vocal folds — are common. The basic list includes vocal nodules, various kinds of polyps, capillary ectasia, epidermoid cyst, mucus retention cyst, glottic sulcus, mucosal bridge, granuloma, scarring, and keratosis. Some of these lesions will resolve with time and medical and/or behavioral (speech pathology) treatment measures – or they will improve to the point that vocal limitations diminish to an acceptable level. Yet others are partly or completely irreversible. In these instances, vocal fold microsurgery may become an option.
Vocal fold granulomas
Most often, this lesion is the result of an endotracheal tube (breathing tube) that was placed for surgery or for respiratory support during a critical illness. At BVI, we believe that these lesions rarely need removal in order to establish a diagnosis; visual criteria for this, along with continued observation, are generally sufficient.
Asymptomatic lesions are observed at intervals to confirm resolution. Symptomatic lesions may be injected with steroid medication in the “chair” in the videoendoscopy procedure room. Only rarely do we go to the operating room – for instance, when a lesion becomes pedunculated (attached by a stalk) but does not seem to want to spontaneously detach in spite of waiting many months.
Cancer of the Larynx and Pharynx
A malignant growth or tumor caused by abnormal, uncontrolled cell division. Local tumors are described as one of the following:
- T1, earliest and smallest (pictured)
- T2
- T3
- T4
Larynx cancer
Dr. Bastian trained with internationally-famous Dr. Joseph Ogura at Washington University in St. Louis. Dr. Richardson received similar training under Dr. George Adams at the University of Minnesota in Minneapolis. Building on that foundation, both physicians have utilized innovative conservation operations for larynx cancer. They have also removed many tumors endoscopically, as inspired by a case Dr. Bastian witnessed as performed by Dr. Wolfgang Steiner, then of Erlangen, now of Gottingen, Germany, in 1983. Using these techniques, surgery can often be a part of patient treatment in a way that preserves voice, swallowing, and breathing function and yet includes what has traditionally been considered the “strong arm” of cancer treatment in this site.
Larynx cancer is a particular interest at our office, where we continue to believe that a true surgical opinion from an individual well-versed in both open conservation and endoscopic laser surgery is critical to the decision-making process and can often provide a very appealing and less morbid option to consider alongside radiation and chemotherapy.
Of special note is Dr. Bastian’s work showing (1) that for early vocal fold cancer, laser excision can provide equal cure rate and voice quality when compared with more traditional radiotherapy and (2) that definitive yet narrow margin excision can be an excellent strategy to “downsize” the size of defects left after cancer extirpation, thereby diminishing voice and swallowing impact, yet with good cure rates.

Recurrent Respiratory Papillomatosis (RRP)
Wart-like lesions in the larynx or trachea, caused by chronic infection with HPV (human papillomavirus).
What is recurrent respiratory papillomatosis (RRP)?
RRP is caused by the human papilloma virus (HPV). In affected individuals, this virus resides chronically in the surface tissue or mucosa of the larynx and may induce proliferation of mucosa (surface tissue) into either low-profile velvety or elevated lesions called papillomas. These lesions can occur on the vocal folds, in areas above the vocal folds, and even in the subglottis and trachea. BVI caseload comprises approximately 140 adult-only patients.
The standard of care for this condition remains periodic vocal fold microsurgery to remove papillomas meticulously but with care to avoid injury to underlying vocal fold structures. BVI physicians have extensive experience over 20 years, with adjuvant treatments, including interferon; the so-called “cabbage pill” (indole 3-carbinol, or its active metabolite marketed as DIM); and most recently, cidofovir, Avastin, and artemisinin. In recent years, we have used cidofovir along with surgery with what seems to be in some cases remarkable clinical success.
Across 20 years, we have had many patients on adjunctive treatments such as interferon, I-3-C, cidofovir, artemisinin, and Avastin. Based upon this experience, we individualize our approach for each patient, but our commonest current methodology is as follows:
New patients–initial “curative” mode. (“Curative” is in quotes to denote a treatment philosophy only, as we of course know that RRP is stubbornly recurrent in most, but not all patients.) We perform meticulous but conservative removal of visible lesions in the operating room, and inject the base with cidofovir or Avastin. When travel logistics allow, we perform two additional injections in the videoendoscopy room of BVI at 3-week intervals, to complete a series of three. On individualized basis, more injections may follow.
Longterm patients with proven and stubbornly recurrent lesions: — “management” mode. Individualization is key, but many opt for periodic pulsed-KTP and/ or Thulium laser treatment in a videoendoscopy procedure room, under topical anesthesia. Hundreds of office-based laser treatments have been performed at BVI during the past 10 years.
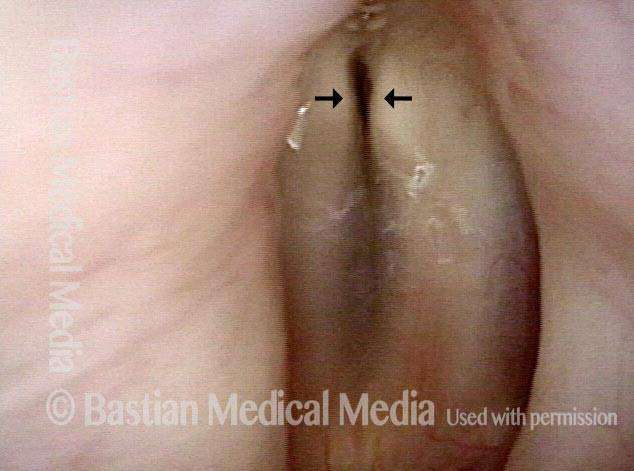
Spasmodic dysphonia (SD)
Neurological disorder in which muscles of the larynx spasm, either choking off or straining the voice or else making it breathy or drop abruptly to a whisper mid-word or sentence:
- Adductory (AD): chokes off or strains
- Abductory (AB): breathy or whispery (pictured)
Our experience with SD patients
The combined experience of Bastian Voice Institute physicians comprises approximately 1500 patients with this rare neurological disorder. We began seeing large numbers of persons with this disorder in 1989, and our patient population continues to come from throughout the United States as well as other countries.
Noteworthy subsets within this SD population include:
- Those whose spasmodic dysphonia is atypical and has therefore been overlooked or misdiagnosed prior to evaluation at Bastian Voice Institute.
- Individuals who have had difficulty achieving consistent results with Botox therapy elsewhere.
- Individuals with abductory spasmodic dysphonia, the injections for which are inherently technically challenging as compared with adductory spasmodic dysphonia.
- Persons with respiratory involvement causing involuntary breath holding or noisy inspiratory sounds as the sole manifestation of laryngeal dystonia, or along with voice manifestations (spasmodic dysphonia).
At BVI, we continue to believe that the mainstay of treatment is Botox therapy. While various surgical approaches to laryngeal dystonia should be a continuing option, the irreversibility, mild unpredictability of surgical results, and potentially evolving nature of any individual’s dystonia manifestations lead us to believe that surgery options should be considered only if optimized Botox therapy results are disappointing. Botox injections are offered weekly at BVI.
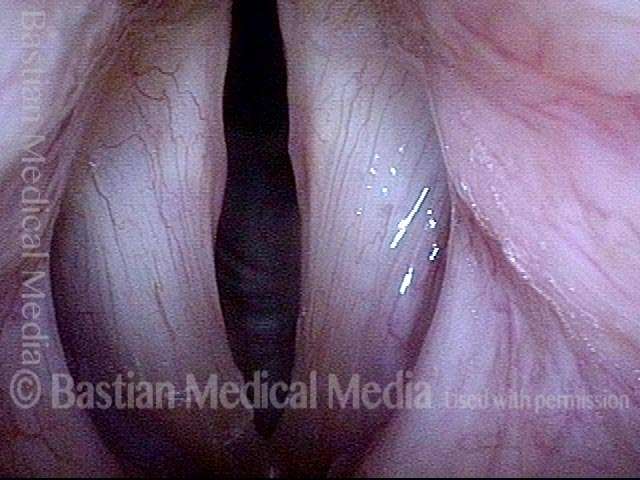
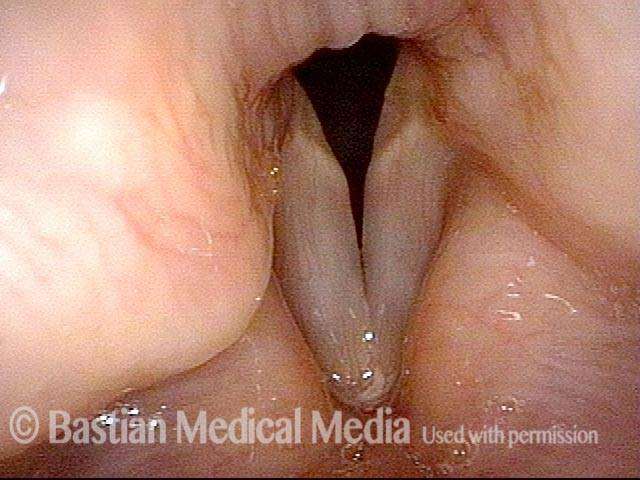
Vocal fold paralysis
Neurological disorder in which one or both vocal folds are paralyzed, causing a weak, breathy voice or difficulty breathing, respectively. Variants include:
- Unilateral paralysis (pictured)
- Bilateral paralysis
- Paresis (weakness, or partial paralysis)
What is vocal fold paralysis?
Vocal fold paralysis and/or paresis (weakness) may be idiopathic (meaning the cause is unknown), presumed to be due to a viral injury after upper respiratory infection; or it may be the result of thyroid, esophageal, lung, heart, or aorta surgery or tumors. Persons with vocal fold paralysis may experience a weak, air-wasting kind of hoarseness. They are unable to compete with background noise; they may also cough on liquids; have a weakened cough; and experience generalized fatigue when they talk for any extended period of time. Particularly when the paralysis seems spontaneous and unexplained, the main diagnostic test, after application of the integrative diagnostic model, is to use radiography –typically a CT scan – to visualize the path of the nerve that goes to the affected vocal fold, to be sure that there is no lesion pressing on the nerve, or other treatable cause of the paralysis.
Treatment for vocal fold paralysis depends upon the severity of vocal limitations, the time since onset of the paralysis, the potential for spontaneous recovery of the paralysis, and patient preference. In some cases this may mean voice building exercises; in others, a temporary gel-consistency implant that is injected into the vocal fold to fatten and firm it up for some months while we await recovery of nerve function.
When the paralysis is known to be permanent, a permanent implant is placed either by injection at BVI, or during an outpatient surgical procedure using a silastic “shim.” BVI physicians manage an estimated 60-plus patients per year with this relatively uncommon problem. About 40 undergo a permanent rehabilitative outpatient surgical procedure called medialization laryngoplasty.
Professional voice disorders
More often than not, the difficulties encountered by professional voice users resolve or diminish to an acceptable level through a combination of medical, speech therapy, and “life strategy” maneuvers. Vocal fold microsurgery (above) is an option for irreversible lesions.

Swallowing Dysfunction
We focus on mouth and throat-related swallowing difficulties, from poor muscular propulsion of food material or from failure of other muscles to relax and let food material pass through:
- Presbyphagia (propulsion)
- Cricopharyngeus dysfunction (non-relaxation), with/without Zenker’s diverticulum (pictured)
Airway Stenosis
Stenosis (narrowing) of the airway at the vocal folds, just below them, or down into the trachea can lead to noisy breathing, reduced exercise tolerance, etc. Causes may include:
- Scarring: post-intubation injury
- Scarring: prior tracheotomy
- Inflammation: Wegener’s granulomatosis (pictured)
What causes scarring of larynx, subglottis, or trachea?
Narrowing or scarring in the airway at the vocal fold level or lower towards the trachea may be caused by external trauma, chemical burn, autoimmune inflammation, endotracheal tube intubation, or tracheotomy. When patients arrive at Bastian Voice Institute, they may be experiencing some degree of exercise intolerance or noisy breathing. In other cases, they are tracheotomy-dependent.
Occasionally a straightforward dilation (stretching) procedure is all that is required to solve the problem; in other instances, reconstructive surgery is necessary to restore or at least improve breathing function. Simple dilation may be done on an outpatient basis during a brief general anesthetic.
Larger reconstructions are done at Advocate Good Samaritan Hospital and typically require a hospital stay of 2—5 days.

Sensory Neuropathic Cough
Variant of chronic cough discovered by Dr. Bastian years ago. A neurogenic cough, often mistakenly thought to be the result of asthma, acid reflux, allergy, or stress/psychological factors.
Non-Organic Disorders
Disorders that arise not from dysfunction of the mechanism itself but instead from how the mechanism is used. These disorders can affect:
- Voice
- Breathing (pictured)
- Coughing
What is a nonorganic voice disorder?
After an upper respiratory infection that never seemed to go away or perhaps because of life stress, some individuals develop a voice disorder that persists in spite of an entirely normal structural and neurological examination.
In this case, the ongoing problem is not based in the larynx itself, but instead in the abnormal use of that mechanism. Sometimes such individuals go for weeks, months, or even years with a distinctly abnormal voice of this sort.
BVI physicians see a large patient population of such individuals from a wide area. Our clinicians’ ability to address the voice’s “skill and will” capabilities and limitations are key to establishing this diagnosis. Sometimes within the first consultation, and almost always by the end of a couple of sessions of voice therapy with one of our recommended speech pathologists, virtually all such patients—assuming appropriate motivation—revert to normal voice on a stable basis.
Want to Learn More?
For a more extensive review of disorders we have treated at BVI, go to Dr. Bastian’s educational multimedia website containing 2,000+ images, videos and audio clips.